- 09/03/2025
- Posted by: Medical Billing Course
- Categories: Medical Billing Career, Medical Billing Certification, Medical Billing Course, Medical Billing Employment, Medical Billing Procedures

Get Certified with Medical Billing & Revenue Cycle Management Training
Every year, healthcare organizations face staggering losses due to billing inefficiencies. You have the power to change that. Our Medical Billing Revenue Cycle Management Training equips you with the skills to make a difference.
Understanding the Impact of Medical Billing
Billions of dollars slip through the cracks annually in healthcare due to inefficient billing practices. This not only affects the financial health of providers but also their ability to deliver top-notch patient care. Accurate billing is more than a necessity—it’s a lifeline. This underscores the critical role of effective Medical Billing Revenue Cycle Management Training in safeguarding healthcare finances.
– American Medical Association
This insight underscores the critical role of effective revenue cycle management in safeguarding healthcare finances.
“Medical billing is the backbone of a thriving healthcare practice. By mastering the intricacies of coding, claims, and reimbursements, you directly contribute to the financial stability that allows providers to focus on what they do best: patient care.” – Tri Smith, Instructor, MedicalBillingCourse.com
With over 5 years of experience as an instructor, Tri has guided thousands of students to successful careers in medical billing, equipping them with the skills and confidence to become certified professionals through our Medical Billing Revenue Cycle Management Training.
Our training in medical billing and revenue cycle management empowers you to process claims with precision, reduce denials, and ensure timely reimbursements. Dive into this guide to discover the essentials of medical billing, explore the revenue cycle stages, learn about certification, understand coding, navigate compliance, start a home-based billing business, and assess job prospects and salary potential. This comprehensive Medical Billing Revenue Cycle Management Training is your pathway to success.
Why Medical Billing Matters in Healthcare
Medical billing translates patient care into standardized codes, submits claims to payers, and tracks reimbursements to maintain cash flow. By converting clinical encounters into CPT, HCPCS, and ICD-10 codes, billers ensure providers are compensated for every service rendered. This is a core component of effective Medical Billing Revenue Cycle Management.
Accurate billing prevents revenue loss, supports financial stability, and enables practices to invest in quality care. Our comprehensive training platform equips you with the skills to excel in these processes and maximize revenue cycle performance through specialized Medical Billing Revenue Cycle Management Training.
The Core of Medical Billing
Medical billing involves a series of interconnected tasks:
- Collecting patient demographics and insurance details.
- Translating treatments and procedures into standardized codes.
- Submitting claims electronically through clearinghouses.
- Following up on unpaid or denied claims.
- Posting payments and reconciling accounts.
These steps form a closed-loop financial system that secures provider revenue and maintains accurate patient records, laying the foundation for effective revenue cycle management.
Boosting Healthcare Revenue Through Efficient Billing
Efficient billing is a direct line to a practice’s financial health by:
- Reducing claim denials with precise code selection.
- Speeding up reimbursement cycles through electronic submissions.
- Enhancing cash flow with accurate payment postings.
- Identifying revenue opportunities through denial analytics.
By minimizing administrative errors, medical billing enhances financial predictability and supports reinvestment in clinical services, driving overall healthcare quality forward. This directly impacts the success of Medical Billing Revenue Cycle Management.
Exploring Types of Medical Billing
Medical billing varies by setting and scope, each requiring specialized skills and processes.
This classification guides billers to adopt specific workflows and compliance protocols, ensuring revenue cycle expertise aligns with organizational needs.
Key Stages of Medical Billing Revenue Cycle Management
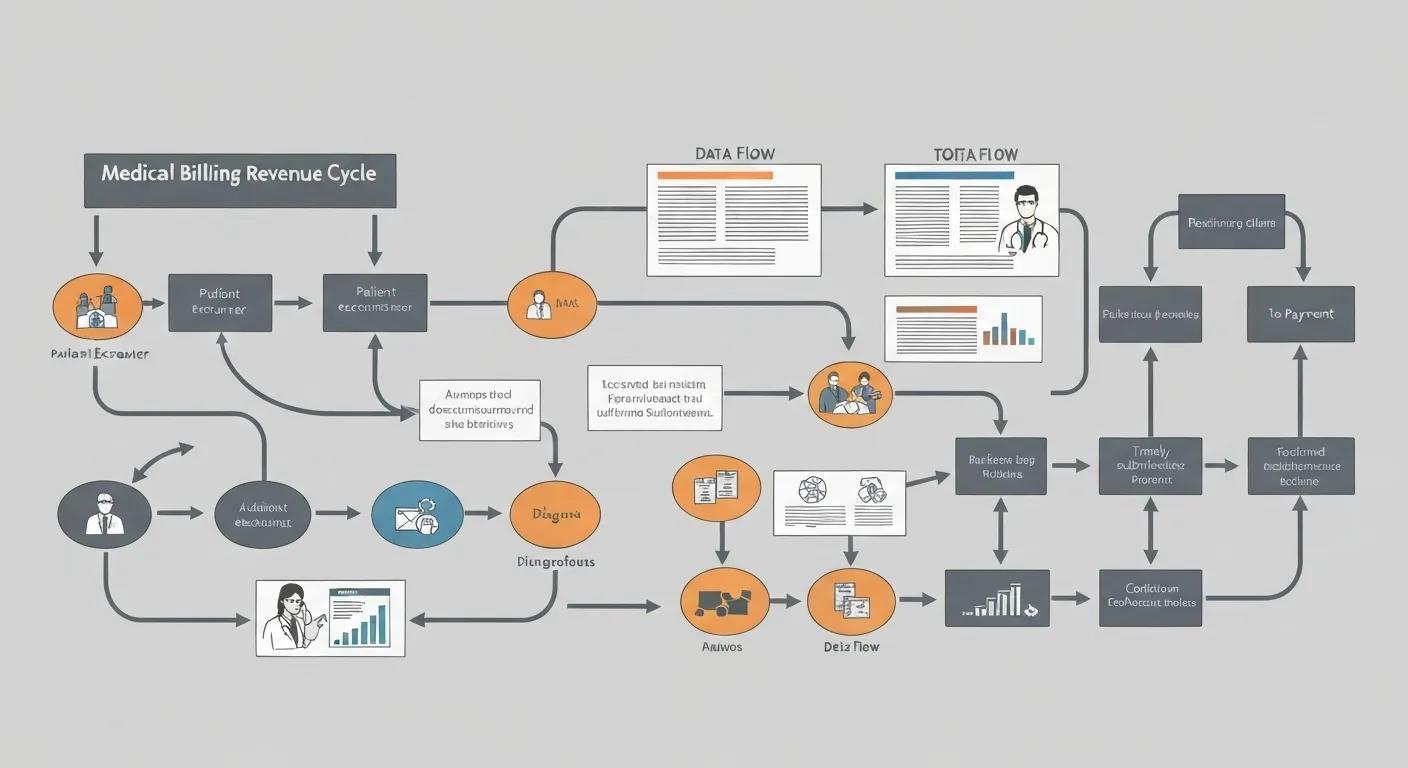
Revenue cycle management (RCM) covers every financial interaction from patient intake to final payment, ensuring providers capture full value for services rendered. Mastery of each stage prevents revenue leakage and accelerates cash flow. Understanding the intricacies of Medical Billing Revenue Cycle Management is crucial for financial health.
Before diving into registration, charge capture, claims, denials, and payment posting, consider how each step secures financial health and supports quality care delivery. Our Medical Billing Revenue Cycle Management Training covers these critical stages in detail.
This structured cycle ensures continuous visibility into financial performance, guiding proactive adjustments that boost revenue integrity.
Starting the Revenue Cycle with Patient Registration
Patient registration kicks off RCM by gathering demographics, insurance coverage details, and authorization information. Verifying insurance eligibility at this stage reduces claim rejections and ensures accurate benefit calculations. Proper registration sets the stage for correct coding and timely payment, preventing revenue delays before they begin.
The Importance of Charge Capture
Charge capture converts clinical services into billable items by assigning appropriate CPT and HCPCS codes. Complete and precise charge capture prevents under-billing, ensures compliance with payer policies, and reduces audits. By capturing every service delivered, practices maintain financial accuracy and uncover revenue opportunities otherwise lost.
Efficient Claims Submission and Processing
Claims submission involves transmitting coded encounters to payers through clearinghouses, which validate data and route errors back for correction. Employing automated clearinghouse interfaces and real-time edit checks expedites processing, reduces manual interventions, and accelerates reimbursement cycles, sustaining provider cash flow.
Best Practices for Denial Management
Denial management identifies reasons for claim denials—such as coding errors or eligibility issues—and implements corrective workflows. A structured approach includes denial tracking, root-cause analysis, timely appeals, and staff training. Effective denial management recovers revenue and refines processes to prevent recurring errors.
Handling Payment Posting in RCM
Payment posting applies remittance advice to patient accounts, reconciling expected revenue with actual received amounts. Automated posting tools and clear reconciliation policies ensure accurate ledger updates, identify underpayments, and flag discrepancies for follow-up, closing the revenue loop.
Becoming a Certified Medical Biller

Certification in medical billing showcases your expertise in coding standards, payer regulations, and RCM processes. It boosts your credibility, enhances job prospects, and justifies higher billing rates. Mastering Medical Billing Revenue Cycle Management is a key outcome of certification.
Our Part 1 course modules cover foundational concepts, while Part 2 delves into the home-based medical billing business model. This is all part of our comprehensive Medical Billing Revenue Cycle Management Training.
Requirements for Certification
Certification typically requires:
- Completion of a recognized training program covering CPT, HCPCS, and ICD-10 coding.
- Passing an exam demonstrating proficiency in coding rules, claim preparation, and compliance.
- Continuing education to maintain credentials and stay current with code updates.
Meeting these requirements validates your capacity to manage billing operations and positions you as a trusted financial steward.
Top Industry Certifications
Leading credentials include:
- CMBP (Certified Medical Billing Professional) – Focus on both physician billing and home business.
- AAPC CPC (Certified Professional Coder) – Focus on physician‐based coding and billing.
- AHIMA CCA (Certified Coding Associate) – Emphasizes inpatient and outpatient coding skills.
- Billing and Coding Specialist (BCS) – Industry‐neutral certification covering end-to-end RCM.
These credentials signal mastery to employers and clients, advancing your career or business prospects.
Duration of Medical Billing Training
Most self-paced online programs span 3–6 months, depending on prior experience and study commitment. Accelerated tracks can be completed in as little as 8–12 weeks, while part-time learners may extend their studies over 6–9 months for deeper practice and review.
Skills Acquired from Medical Billing Courses
Medical billing courses develop skills in:
- Medical coding (CPT, HCPCS, ICD-10)
- Claims processing and clearinghouse interfaces
- Denial review and appeals management
- Patient billing inquiries and account reconciliation
These competencies equip you to drive revenue performance and implement efficient billing workflows.
The Role of Medical Coding in Revenue Cycle Management
Medical coding translates clinical documentation into standardized code sets, forming the backbone of accurate billing and revenue optimization. By assigning precise codes, coders enable correct claim adjudication and compliant reimbursement. This is fundamental to successful Medical Billing Revenue Cycle Management.
Understanding each coding system deepens your capacity to spot errors, reduce denials, and enhance practice profitability. Our Medical Billing Revenue Cycle Management Training emphasizes the critical role of coding.
The Importance of CPT Coding
CPT (Current Procedural Terminology) coding categorizes medical procedures and services into five-digit numeric codes maintained by the AMA. Accurate CPT coding ensures providers are reimbursed for the exact services rendered and supports performance analytics for clinical quality and financial planning.
HCPCS Coding in Medical Billing
HCPCS (Healthcare Common Procedure Coding System) complements CPT codes by covering supplies, equipment, and certain services not found in CPT. Level II HCPCS codes track durable medical equipment, while Level I codes align with CPT, together providing comprehensive service representation.
The Role of ICD-10 Coding in Billing Accuracy
ICD-10 (International Classification of Diseases, Tenth Revision) codes classify diagnoses and health conditions. Linking ICD-10 codes with CPT procedures demonstrates medical necessity to payers, reducing denials and justifying treatments rendered during patient encounters.
Enhancing Your Career with Coding Certifications
Coding certifications—such as CPC, CCA, and CCS—validate your mastery of code sets and regulations. Certified coders command higher salaries, gain access to specialized roles in hospitals and billing firms, and contribute to lowering denial rates through precise code selection.
Compliance in Medical Billing
Compliance in medical billing upholds patient privacy, data security, and ethical billing practices. Adhering to regulations protects providers from audits, fines, and reputational harm while fostering patient trust. Proper compliance is a cornerstone of robust Medical Billing Revenue Cycle Management.
Key regulations shape billing protocols and operational controls throughout the revenue cycle. Our Medical Billing Revenue Cycle Management Training ensures you are well-versed in these critical areas.
HIPAA Compliance in Medical Billing
HIPAA mandates standards for protecting patient health information during billing and claims transmission. Secure handling of electronic transactions and proper authorization for disclosure reduce breach risk and maintain patient confidentiality.
HIPAA Compliance in Medical Billing
HIPAA mandates standards for protecting patient health information during billing and claims transmission. Secure handling of electronic transactions and proper authorization for disclosure reduce breach risk and maintain patient confidentiality.
– U.S. Department of Health & Human Services
This citation supports the article’s discussion on compliance requirements in medical billing, specifically focusing on HIPAA regulations.
Fraud and Abuse Prevention Strategies
Preventing fraud and abuse involves:
- Verifying medical necessity before coding.
- Implementing audit trails for all billing changes.
- Conducting regular internal reviews of high-risk claims.
- Training staff on false claims and anti-kickback statutes.
These measures deter improper billing and safeguard organizational integrity.
The OIG Work Plan’s Influence on Billing Practices
The OIG (Office of Inspector General) publishes an annual work plan identifying areas of high audit risk, such as telehealth claims or unbundling. Aligning billing protocols with OIG priorities helps preempt audits and ensures billing integrity.
Other Essential Regulations for Medical Billers
Beyond HIPAA and OIG guidance, billers must understand:
- CMS National Coverage Determinations.
- State Medicaid billing rules.
- Payer-specific fee schedules.
- Stark Law and Anti-Kickback Statute implications.
Staying current with these regulations ensures compliant billing and minimizes liability.
Starting a Home-Based Medical Billing Business

Launching a home-based medical billing business offers flexibility, scalability, and strong income potential. By combining certification with entrepreneurial know-how, you can serve multiple healthcare providers and control your own schedule. Effective Medical Billing Revenue Cycle Management is key to client success.
Our advanced revenue cycle management modules teach both technical and business skills to prepare you for independent practice. This is a crucial component of our Medical Billing Revenue Cycle Management Training.
Steps to Launch Your Medical Billing Business
To establish your practice:
- Register your business entity and obtain any required licenses.
- Secure reliable medical billing software and EHR integrations.
- Develop service agreements and fee structures.
- Market your services to physician offices, clinics, and therapists.
- Implement policies for data security, billing protocols, and client communication.
These steps provide a roadmap for a compliant, profitable billing venture.
Creating a Medical Billing Business Plan
A robust plan outlines the following:
- Target market and competitive analysis.
- Service offerings and pricing model.
- Marketing and sales strategies.
- Financial projections for revenue, expenses, and cash flow.
- Operational workflows and quality control measures.
A clear business plan attracts clients and guides sustainable growth. Here’s a resource for essential things to keep in your remote office.
Software and Technology for Home-Based Billing
Essential tools include:
- Practice management systems for scheduling and reporting.
- Clearinghouse integrations for electronic claim submission.
- Secure portals for patient statements and payment processing.
- Cloud-based EHR platforms for documentation exchange.
Selecting interoperable, scalable software streamlines RCM and enhances client satisfaction.
Marketing Your Medical Billing Services
Effective marketing tactics involve:
- Building a professional website with service descriptions.
- Networking with local healthcare associations.
- Offering free consultations or audits.
- Showcasing case studies of revenue gains.
- Leveraging social media and online review platforms.
Consistent outreach and proven results establish credibility and drive client acquisition.
Job Outlook and Salary Potential for Medical Billers
The demand for skilled medical billers and coders is rising as practices seek to optimize revenue and comply with evolving regulations. According to the U.S. Bureau of Labor Statistics, employment of medical records specialists is projected to grow 7% from 2022 to 2032, outpacing average occupational growth. Expertise in Medical Billing Revenue Cycle Management is highly sought after.
Job Outlook for Medical Records Specialists
The U.S. Bureau of Labor Statistics projects a 7% growth in employment for medical records specialists from 2022 to 2032, which is faster than the average for all occupations. This growth is driven by the increasing complexity of healthcare regulations and the need for accurate medical billing and coding.
– U.S. Bureau of Labor Statistics
This citation provides the job outlook and salary potential for medical billers, as mentioned in the article.
As automation and AI reshape RCM, professionals with advanced analytics and coding skills will command premium rates, ensuring continued career advancement.
Current Demand for Medical Billing Professionals
Healthcare’s shift toward value-based care and telehealth has expanded billing requirements, generating new coding and reimbursement challenges. Practices rely on certified billers to navigate complex regulations and optimize financial outcomes.
Earnings Potential for Certified Medical Billers
Certified billers typically earn 10–20% more than non-certified peers. With specialized credentials and denials expertise, top performers can exceed $60,000 annually, especially in high-cost markets or niche specialties.
Emerging Trends in Medical Billing Careers
Key trends include:
- Increased use of AI for code validation and denial prediction.
- Integration of telehealth and remote monitoring codes.
- Data analytics for revenue forecasting and performance optimization.
Staying ahead of these trends deepens your expertise and differentiates your services.
Advancing Your Career Through Continuing Education
Ongoing training in advanced coding, payer policy updates, and RCM analytics ensures you remain competitive. Courses on emerging topics, such as AI in medical billing or advanced denial prevention, prepare you for leadership roles and higher compensation.
“Before taking the medical billing course, I was struggling to find a stable career path. The comprehensive training provided me with the essential skills and confidence to not only pass my certification exam but also to land a great job as a medical biller. I’m now earning a comfortable salary and have a clear path for career advancement.” – Sarah K.
Read more success stories from our graduates and see how they transformed their careers. Explore our success stories.
Mastering medical billing and revenue cycle management underpins healthcare’s financial health and opens rewarding career and business opportunities. By understanding essential concepts, completing certification, leveraging coding systems, adhering to compliance, and applying entrepreneurial strategies, you position yourself as an indispensable partner to providers. Visit our programs and take the next step toward becoming a certified medical biller and launching a thriving medical billing business today.

