- 01/12/2026
- Posted by: Medical Billing Course
- Category: Medical Billing Course

Master Advanced Billing Techniques for Medical Success: Your Comprehensive Guide
Unlock peak efficiency, slash claim rejections, and boost your medical practice’s revenue by up to 30% in just six months with advanced billing techniques. This guide provides practical strategies across revenue cycle optimization, compliance mastery, technology integration, and entrepreneurial growth to ensure your practice thrives. Discover how advanced billing enhances cash flow, minimizes operational risks, and paves the way for certification and business ownership. We’ll cover:
- The core principles of advanced medical billing and essential foundational skills
- Proven strategies for optimizing your entire revenue cycle
- Critical compliance requirements under HIPAA and various payer regulations
- How AI, automation, and software integration are revolutionizing billing
- The essential steps to launch, market, and grow a home-based billing business
- Key trends shaping the future, including value-based care, outsourcing, and patient-centric models
- The career advantages, salary expectations, and remote work opportunities available
What Are Advanced Medical Billing Techniques and Why Are They Essential?
Advanced medical billing techniques involve sophisticated claim adjudication, proactive denial management, and insightful analytics to expedite reimbursements and improve financial performance. By implementing specialized workflows, such as payer-specific coding edits and automated claim scrubbing, practices can significantly reduce unpaid claims and strengthen cash flow.
“The complexity of modern healthcare demands more than just basic claim submission. Advanced billing isn’t merely about processing; it’s about strategic financial management that directly impacts patient care and practice sustainability.” – Tri Smith, Instructor, MedicalBillingCourse.com
These methods are crucial because they:
- Minimize Denials through real-time error detection and correction
- Accelerate Payments by ensuring optimized and accurate claim submissions
- Enhance Reporting capabilities with robust revenue cycle analytics
- Support Compliance by rigorously applying advanced coding rules and regulations
Impact of Advanced Billing Techniques
Advanced medical billing techniques, incorporating sophisticated claim adjudication and proactive denial management, can dramatically enhance financial outcomes for medical practices. These methods, including payer-specific coding edits and automated claim scrubbing, are instrumental in reducing unpaid claims and improving cash flow, ultimately leading to a more robust revenue cycle.
This research validates the article’s assertions regarding the advantages of advanced billing techniques.
Embracing these advanced skills not only protects your practice’s revenue but also prepares billing professionals for higher levels of certification. To further elevate your expertise, explore how the Medical Billing Course Program – Part 2 builds upon foundational knowledge with cutting-edge methodologies.
How Do Advanced Billing Techniques Improve Medical Practice Revenue?
Advanced billing techniques boost revenue by proactively identifying potential claim errors, streamlining the appeals process, and leveraging data insights to correct systemic issues that lead to denials. Real-time claim scrubbing flags incomplete or incorrect information before submission, while automated appeal workflows ensure that denied claims are promptly resubmitted. Collectively, these efforts can achieve:
- A 25–30% reduction in claim denial rates
- A 20% acceleration in the reimbursement cycle
- Improved net collection rates by prioritizing high-value claims
Reducing manual rework allows your staff to dedicate more time to patient engagement and strategic practice growth, reinforcing the practice’s financial stability and operational resilience.
What Key Skills Define Advanced Medical Billing?
Advanced medical billing demands a combination of technical proficiency and analytical acumen that goes beyond basic claim entry. Essential skills include:
- Expert command of CPT, ICD-10, and HCPCS coding standards
- Deep understanding of payer-specific billing guidelines and contract stipulations
- Advanced proficiency in denial analysis and effective appeals management
- The ability to interpret key RCM metrics and utilize dashboard analytics
- Familiarity with critical compliance frameworks such as HIPAA and OIG regulations
This comprehensive skill set empowers billers to expertly navigate complex claim scenarios, maintain consistent cash flow, and advance their careers toward certification and professional growth.
How Does Certification Enhance Mastery of Advanced Billing?
Certification serves as definitive proof of your mastery of advanced billing techniques, showcasing your competence in industry-recognized standards like the Certified Professional Biller (CPB) or CBCS credentials. Certified professionals consistently achieve higher collection rates and benefit from:
- Average salaries that are 27% higher than their non-certified counterparts
- Recognition as a trusted authority in healthcare revenue management
- Enhanced employability and greater access to remote work opportunities
Benefits of Certification
Certification in advanced billing not only validates your expertise but also typically leads to higher salaries and expanded career opportunities. Certified professionals are widely recognized as trusted experts in healthcare revenue management, which significantly boosts career prospects and earning potential.
This citation supports the article’s discussion on the significant advantages of obtaining certification in medical billing.
Earning certification through our comprehensive curriculum ensures you’re equipped to apply best practices in real-world scenarios, accelerating both your personal career trajectory and your practice’s success.
How Can You Optimize Revenue Cycle Management for Medical Success?

Optimizing revenue cycle management (RCM) requires a strategic orchestration of every stage, from initial patient registration to the final payment, to maximize efficiency and minimize revenue leakage. By standardizing processes, implementing robust denial prevention strategies, and diligently monitoring key performance indicators, practices can achieve sustainable financial health.
What Are the Best Practices for Denial Management Strategies?
Effective denial management begins with accurately classifying denials by their root cause and implementing targeted, efficient appeals workflows. Key best practices include:
- Prioritizing denials based on urgency and value to address high-impact claims first.
- Utilizing pre-designed, automated appeal templates that align with specific payer requirements.
- Consistently tracking denial reasons to inform coding education and drive process improvements.
A focused denial management strategy significantly reduces recurring errors and shortens the turnaround time for claim resubmissions, leading to recovered revenue and more predictable cash flow.
How to Manage Accounts Receivable and Payment Posting Efficiently?
Efficient accounts receivable (AR) management is critical for ensuring timely payment posting and accurate financial reconciliation. Essential steps include:
- Posting remittance advice daily to promptly update patient and payer balances.
- Implementing automated follow-up queues for outstanding AR across aging buckets.
- Conducting routine audits to verify the accuracy of posting and identify any discrepancies.
This structured approach maintains clean financial ledgers and accelerates cash collections, reinforcing the stability of your revenue cycle.
Which Tools and Metrics Help Track Revenue Cycle Performance?
Monitoring RCM performance effectively relies on clearly defined metrics and intuitive software dashboards that highlight trends and pinpoint bottlenecks. The following table outlines critical performance indicators:
| Metric | Definition | Benchmark |
|---|---|---|
| Days in Accounts Receivable | The average number of days it takes to collect payment | Under 45 days |
| Clean Claim Rate | The percentage of claims paid upon their initial submission | 95% or higher |
| Denial Rate | The percentage of claims that are denied by payers | Under 5% |
| Net Collection Rate | The percentage of expected reimbursement that is actually collected | 98% or higher |
Diligent tracking of these metrics empowers data-driven decision-making and facilitates continuous improvement across all revenue cycle workflows.
How Do Regulatory Compliance and HIPAA Impact Advanced Medical Billing?
Advanced medical billing practices must strictly adhere to federal regulations, including HIPAA’s privacy and security rules, to safeguard patient data and prevent costly penalties. Compliance frameworks also guide ethical billing practices and reinforce essential fraud prevention measures.
What Are Advanced HIPAA Compliance Requirements for Medical Billers?
For advanced billers, HIPAA compliance involves implementing stringent controls over the access, transmission, and storage of electronic protected health information (ePHI). Key requirements include:
- Ensuring ePHI is encrypted both when stored and during transmission.
- Implementing role-based access controls to strictly limit data exposure.
- Maintaining regular audit logs to monitor and review all system access activities.
Adherence to these standards not only protects patient trust but also ensures the uninterrupted flow of revenue. For a comprehensive understanding of HIPAA protocols, consult our Medical Billing Course Program – HIPAA Compliance.
How to Prevent Fraud and Abuse in Medical Billing?
Preventing fraud and abuse in medical billing hinges on establishing robust internal controls, providing thorough staff training, and conducting proactive audits. Core strategies include:
- Meticulously verifying service documentation against all coding entries.
- Performing periodic, random audits of all submitted claims.
- Establishing clear escalation workflows for any suspected irregularities.
Implementing strong anti-fraud measures protects practices from legal liabilities and maintains positive payer relationships.
What Are Payer-Specific Regulations and Their Billing Implications?
Every insurance payer maintains unique claim adjudication rules and specific documentation standards. Effectively navigating these variations requires:
- Maintaining an up-to-date payer policy matrix detailing current guidelines.
- Customizing claim edits and appeal letters to meet specific payer requirements.
- Leveraging payer portals for direct and efficient error resolution.
Tailoring billing processes to precisely match payer policies significantly increases first-pass claim acceptance rates and minimizes denials.
How Is Technology Transforming Advanced Medical Billing Techniques?
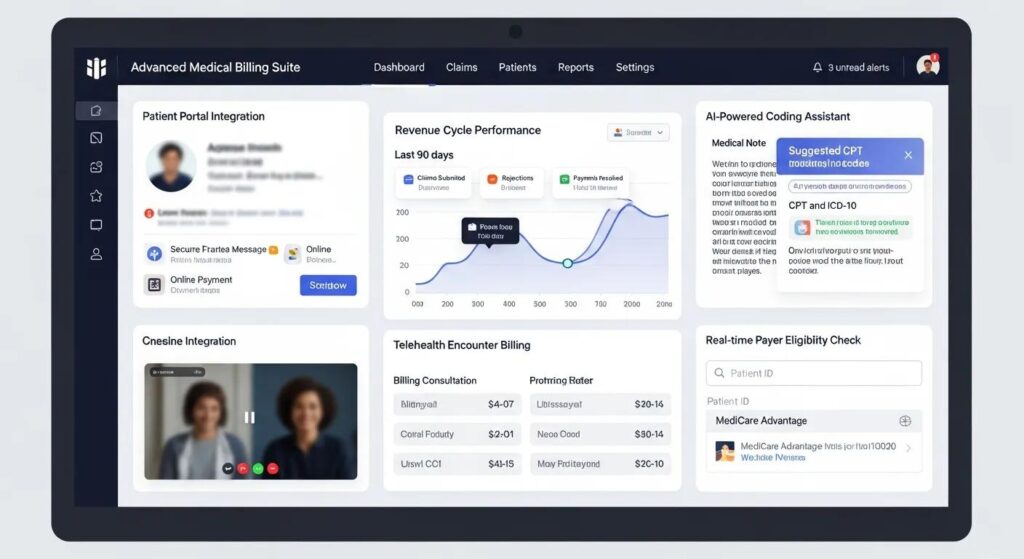
Technology empowers billers to automate repetitive tasks, apply intelligent edits, and analyze extensive claim datasets for continuous improvement. The integration of digital tools significantly boosts accuracy and enhances staff productivity.
What Role Does AI and Automation Play in Medical Billing?
AI and automation streamline the entire claim processing workflow by:
- Identifying claim errors with machine-learning-powered claim scrubbing.
- Generating customized appeal letters based on specific denial reason codes.
- Automating the process of payment posting and financial reconciliations.
These intelligent workflows reduce manual effort, improve billing accuracy, and have the potential to decrease denial rates by as much as 30 percent.
How to Integrate EHR/EMR Systems with Medical Billing Software?
Seamless EHR/EMR integration eliminates data silos and ensures a consistent flow of patient and encounter information into billing systems. Key integration steps include:
- Accurately mapping clinical encounter fields to the corresponding billing software charge entries.
- Configuring bi-directional interfaces to facilitate efficient eligibility verification.
- Thoroughly testing end-to-end transactions to validate data integrity and accuracy.
A well-integrated system accelerates claim submission processes and enhances compliance with essential documentation requirements.
What Features Should You Look for in Medical Billing Software?
When evaluating medical billing platforms, prioritize capabilities that actively support advanced workflows. The table below highlights essential features to consider:
| Software Feature | Function | Benefit |
|---|---|---|
| Automated Claim Scrubbing | Applies rule-based edits prior to claim submission | Minimizes denials and reduces rework efforts |
| AI-Driven Analytics | Generates comprehensive revenue cycle performance reports | Identifies key trends and areas for improvement |
| EHR/EMR Interface | Synchronizes patient and encounter data seamlessly | Ensures accurate charge capture and billing |
| Cloud-Based Architecture | Provides scalable, secure access from anywhere | Facilitates remote work and team collaboration |
Selecting software equipped with these advanced features future-proofs your billing operations and supports scalable business growth.
How Can You Start and Scale a Successful Home-Based Medical Billing Business?
Launching a home-based medical billing service offers significant entrepreneurial opportunities and flexible work arrangements. A well-defined business plan, targeted marketing efforts, and a commitment to quality service delivery are fundamental to success.
What Are the Steps to Launch a Home-Based Medical Billing Service?
To successfully start your own medical billing practice, follow these essential steps:
- Develop a Comprehensive Business Plan outlining your services, pricing structure, and target market.
- Obtain Professional Certification from a recognized program to establish credibility and expertise.
- Invest in Robust Billing Software and secure necessary EHR/EMR integration tools.
- Register Your Business Entity and ensure full compliance with all HIPAA requirements.
- Build Efficient Operational Workflows for claim submission, denial management, and reporting.
Each of these steps is crucial for laying a solid foundation for professional service delivery and ensuring client satisfaction.
How to Acquire and Retain Clients for Your Billing Business?
Client acquisition and retention strategies are built on demonstrating expertise, unwavering reliability, and clear, consistent communication. Effective tactics include:
- Showcasing proven success stories and client testimonials, visit Medical Billing Success Stories for examples.
- Offering complimentary workflow assessments to pinpoint potential billing inefficiencies.
- Providing transparent reporting dashboards that clearly display key performance metrics.
Consistently delivering high-quality service and engaging in proactive outreach fosters strong, long-term client partnerships.
What Strategies Help Scale and Grow Your Medical Billing Practice?
Scaling your medical billing practice effectively involves diversifying services, refining operational processes, and leveraging strategic partnerships. Key strategies include:
- Expanding service offerings into niche medical specialties with tailored billing protocols.
- Outsourcing routine administrative tasks to specialized teams to enhance efficiency.
- Implementing robust referral programs and actively engaging in industry networking.
Focusing on scalability positions your business for sustainable growth and increased profitability.
What Are the Emerging Trends and Future Outlook in Advanced Medical Billing?
The medical billing landscape is continuously evolving, with value-based care models, increased automation, and patient-centric approaches significantly reshaping how services are reimbursed and delivered. Staying informed about these emerging trends is crucial for maintaining long-term relevance and identifying new revenue opportunities.
How Is Value-Based Care Changing Medical Billing Models?
Value-based care fundamentally shifts reimbursement from a volume-based system to one focused on quality metrics, requiring billers to:
- Accurately track outcome-based performance indicators.
- Meticulously document care coordination and patient engagement activities.
- Align billing codes precisely with quality measure reporting requirements.
This significant transformation emphasizes preventive services and a more holistic approach to revenue cycle management.
What Impact Will AI and Automation Have on Future Billing Practices?
AI and robotic process automation are poised to further minimize manual effort, with projections indicating that approximately 85 percent of claims will involve automation by 2025. These advanced technologies will:
- Provide predictive analytics to forecast potential denial risks proactively.
- Automate routine audit procedures and compliance checks.
- Enable real-time financial reporting for more informed, proactive decision-making.
Embracing automation strategically positions practices to excel in a rapidly evolving, high-volume billing environment.
How Are Outsourcing and Patient-Centric Billing Shaping the Industry?
Outsourcing billing functions to specialized, expert providers offers significant cost savings and allows practices to maintain a sharper focus on core operations. Simultaneously, patient-centric billing models prioritize:
- Transparent invoicing that provides clear breakdowns of services rendered.
- Flexible payment options and convenient digital payment solutions.
- Dedicated support channels to address patient inquiries efficiently.
Collectively, these approaches enhance patient satisfaction and contribute to more stable practice revenue streams.
What Career Benefits and Salary Expectations Come with Mastering Advanced Billing Techniques?
Mastering advanced billing techniques unlocks higher earning potential, opens doors to diverse career paths, and offers the flexibility of remote work. Achieving certification and developing deep domain expertise translates directly into tangible professional rewards.
How Does Certification Affect Medical Biller Salary and Job Opportunities?
Certification significantly enhances your market value by demonstrating proven proficiency in complex billing workflows. Certified medical billers typically earn:
- An average hourly wage of approximately $30.14, compared to about $25.84 for non-certified peers.
- Salaries that are, on average, 27 percent higher across various industry roles.
- Greater access to remote positions, specialized consultancy roles, and leadership opportunities.
Certification acts as a catalyst for accelerated career growth and broadens your job prospects within hospitals, private practices, and third-party billing service bureaus.
What Is the Job Outlook for Advanced Medical Billing Professionals?
The U.S. Bureau of Labor Statistics forecasts approximately 8 percent job growth for medical billing specialists between 2022 and 2032, driven by increasing healthcare demand and growing regulatory complexity. This projected growth translates to nearly 15,000 annual job openings, underscoring the strong market demand for skilled billing professionals.
Job Outlook for Medical Billing Professionals
The U.S. Bureau of Labor Statistics projects an 8 percent growth rate for medical billing positions from 2022 to 2032, fueled by rising healthcare demand and increasing regulatory complexity. This growth indicates a robust market demand for proficient medical billers.
- U.S. Bureau of Labor Statistics
This data supports the article’s claims regarding the positive job outlook for medical billing professionals.
Can Medical Billers Work Remotely and What Are the Benefits?
Absolutely, remote medical billing has become a widely accepted and standard work arrangement, offering numerous advantages such as:
- Flexible scheduling options that promote better work-life balance
- Reduced commuting expenses and lower overhead costs
- Access to a broader client base without geographical limitations
Remote work arrangements empower certified professionals to deliver expert billing services effectively from virtually any location.
Mastering advanced billing techniques is key to elevating practice revenue, ensuring compliance, and opening pathways to valuable certification and entrepreneurial ventures. By honing your skills in denial management, leveraging automation effectively, and adhering strictly to regulatory standards, you position both yourself and your practice for sustained financial success. The Medical Billing Course – Home provides comprehensive training and dedicated support to guide you through every advanced method, from technical proficiency to successful business launch. Start implementing these strategies today to transform your billing operations and achieve lasting medical success.
About the Author
Tri Smith is a dedicated Instructor at MedicalBillingCourse.com, bringing over five years of invaluable experience in guiding students toward earning their medical billing certification. Committed to supporting learners from all backgrounds, Tri empowers graduates to translate their training into tangible career opportunities. His expertise helps students navigate pathways to successful remote billing roles and even launch their own thriving home-based medical billing businesses, ensuring they are well-equipped for the evolving demands of the healthcare industry.

